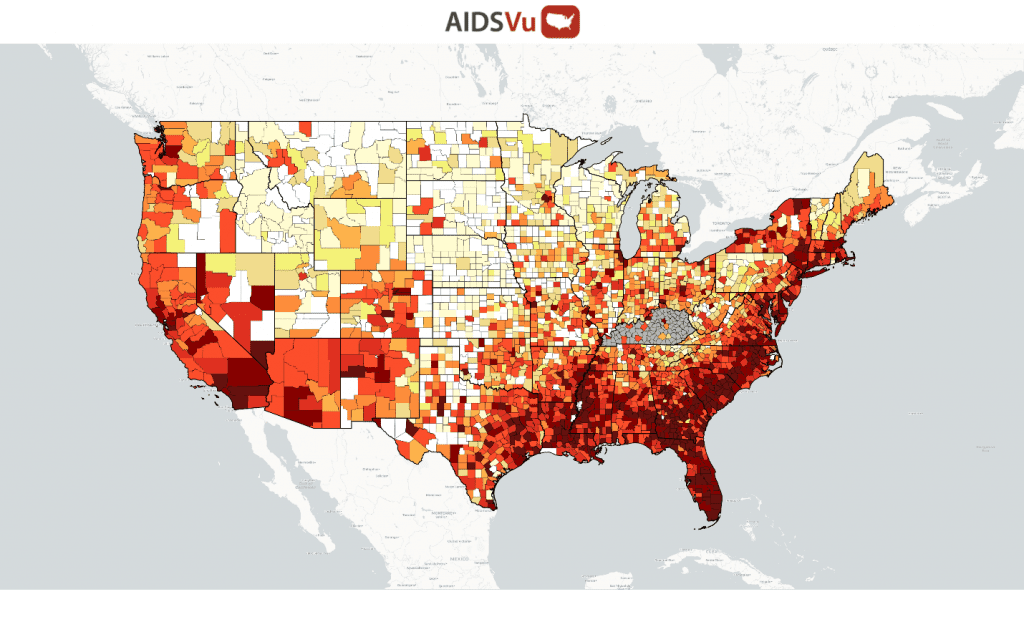
Fig -New HIV Diagnoses 2018 – from AIDSVU
![]()
This is the 40th year of the AIDS epidemic. Older Adults with HIV account for over 50% of the total HIV population in the USA. In some urban localities, they represent 60-65% of those living with HIV. The number of people living with HIV has increased to nearly 1.2 million, including those who are undiagnosed. This is an increase over the period of 2009 to 2018 from nearly 800,000. These increases are a result of better ART therapy, better adherence to ART medication and new HIV cases. In 2019 there were nearly 35,000 new HIV diagnoses. This is a marked reduction in new HIV diagnoses from about 45,000 in 2009.
The number of new diagnoses in those 50 years and older has persisted at about one in six. In 2019, there were just over 6000 new HV diagnoses in older adults. For all ages in the subgroup of men who have sex with men (MSM) there was an overall decrease in the number of cases for white MSM with no change in Black MSM and increases seen for Hispanic and Asian MSM. However, the good news is that the improvement of HIV therapy during this period has resulted in longer life expectancy. For many, that life expectancy is the same as seen in those without HIV infection,
There are various factors- such as age, ethnicity, and race- that affect the frequency of HIV in various parts of the country. Initially, the epidemic occurred in the larger cites near the east and west coasts. Now the major concentrations are occurring in the south (See figures below). For example, it is estimated that 52% of the new HIV cases occur in the southern part (i.e. Deep South) of the country. The reasons for these higher rates in occurrence are not totally clear. One of the likely factors is the larger rural regions found in the Deep South. Rural areas are more likely to not have access to skilled HIV care physicians and nurses as well as hospitals or clinics. This is true for both prevention and treatment of HIV. In rural areas, a visit to a doctor’s office can be challenging. Also, many of the states do not support additional care covered by Medicaid. Similarly, access to PrEP for prevention has been difficult to implement in the Deep South. The increased rates of HIV infections in the south among those aged 25-34 reflect a reluctance to discuss sex with their care providers, high levels of homophobia and other stigmas, as well as poor health literacy.
Older adults with and without HIV face these same challenges of access to care and persistent stigma. To address these challenges, there have been attempts to improve public health surveillance systems and increase efforts to reach out to those at risk with more testing and care. For those reluctant to talk about sexual health- which often include the at-risk seniors- with their doctors, there has been an expansion of telehealth efforts with independent staff and mail services. Fortunately, more financial resources from the federal government have been made available to the states with high HIV rates There is more optimism that various goals to reduce the frequency of new cases and treat those in the south will likely define the next decade of the HIV epidemic.
Patrick S Sullivan, et al. (2021) Epidemiology of HIV in the USA: epidemic burden, inequities, contexts, and responses. The Lancet Vol 397 March 20, 2021 pp 1095-1106